As a physician who has witnessed the devastating toll of tobacco firsthand, both in bustling city hospitals and remote clinics during my travels, I feel compelled to share the stark medical realities of smoking. It’s not just a bad habit; it’s a complex addiction driving a cascade of biological destruction. Understanding these hazards from a medical perspective is the first crucial step towards reclaiming your health and embracing a smoke-free life – essential for anyone wanting to fully experience the vitality travel demands.

Beyond the Lungs: The Systemic Onslaught of Smoke
Cigarette smoke is a toxic cocktail of over 7,000 chemicals, including at least 70 known carcinogens. Its damage is far-reaching:
1. Cardiovascular Catastrophe:
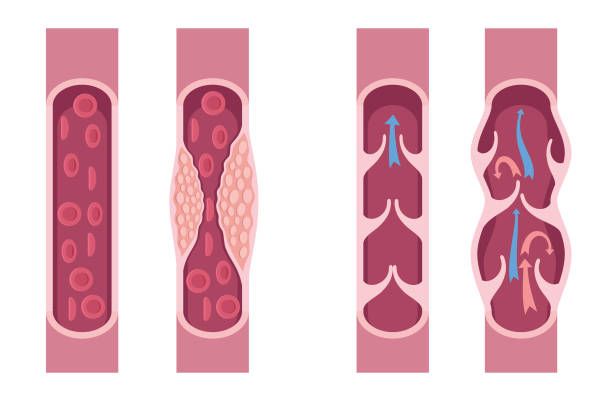
- Atherosclerosis: Nicotine and other toxins damage the delicate endothelial lining of arteries. This allows LDL (“bad”) cholesterol to infiltrate the arterial wall, triggering inflammation and plaque buildup. This narrows arteries, restricting blood flow.
- Hypertension: Nicotine is a potent vasoconstrictor, causing arteries to tighten, forcing the heart to work harder and raising blood pressure.
- Increased Clotting: Smoking makes platelets stickier and increases fibrinogen levels, significantly raising the risk of dangerous blood clots.
- Coronary Heart Disease (CHD): The leading cause of death among smokers. Plaque buildup in coronary arteries starves the heart muscle of oxygen, causing angina (chest pain) and heart attacks.
- Stroke: Plaque in carotid arteries or clots traveling to the brain cause ischemic strokes. Smoking also increases the risk of hemorrhagic stroke (bleeding in the brain) by weakening blood vessels.
- Peripheral Artery Disease (PAD): Reduced blood flow to limbs, causing pain (claudication), poor wound healing, infections, and potentially gangrene and amputation.
2. Respiratory Ruin:

- Chronic Obstructive Pulmonary Disease (COPD): An umbrella term encompassing emphysema and chronic bronchitis. Smoke destroys lung elasticity (emphysema) and inflames airways, causing excessive mucus and chronic cough (bronchitis). This leads to progressive, irreversible shortness of breath – a thief of vitality.
- Lung Cancer: The most infamous hazard. Carcinogens like benzopyrene cause DNA mutations in lung cells, leading to uncontrolled growth. Smoking is responsible for about 85% of lung cancer cases.
- Increased Infections: Smoke paralyzes and damages the cilia (tiny hairs) that clear mucus and pathogens from the airways. This makes smokers far more susceptible to pneumonia, influenza, and tuberculosis.
- Asthma Exacerbation: Smoke is a potent trigger for asthma attacks and worsens overall control.
3. Cancer Beyond the Lungs: Smoking is a major risk factor for cancers of the:
- Mouth, Throat (Pharynx & Larynx)
- Esophagus
- Stomach
- Pancreas
- Liver
- Kidney & Bladder
- Cervix
- Colon & Rectum
- Acute Myeloid Leukemia (AML)

4. Reproductive and Developmental Damage:
- Men: Reduced sperm count, increased sperm abnormalities, erectile dysfunction (due to vascular damage).
- Women: Reduced fertility, earlier menopause, increased risk of cervical cancer. During pregnancy: increased risk of miscarriage, stillbirth, preterm birth, low birth weight, placental problems (placenta previa, abruption), and sudden infant death syndrome (SIDS).
5. Accelerated Aging & Other Impacts:
- Skin: Premature wrinkles, sagging, yellowing due to impaired blood flow and collagen/elastin breakdown.
- Eyes: Increased risk of cataracts and age-related macular degeneration (AMD), leading causes of blindness.
- Bones: Increased risk of osteoporosis and fractures due to reduced bone density.
- Immune System: Chronic inflammation and impaired immune function.
- Diabetes: Increases insulin resistance and the risk of developing Type 2 diabetes; makes existing diabetes harder to control.
- Oral Health: Gum disease (periodontitis), tooth loss, stained teeth, oral cancers.
The Addicted Brain: Why Quitting is Tough (But Not Impossible)
Nicotine is highly addictive, acting on the brain’s reward pathways. It stimulates the release of dopamine, creating feelings of pleasure and reinforcement. Over time, the brain adapts, needing more nicotine to achieve the same effect (tolerance) and causing unpleasant withdrawal symptoms (irritability, anxiety, difficulty concentrating, cravings, restlessness) when nicotine levels drop. This powerful neurobiological cycle makes quitting challenging, but absolutely achievable with the right strategies.
Prescribing Freedom: Evidence-Based Strategies to Quit Smoking
Quitting is the single most important step a smoker can take for their health. Benefits begin within hours and continue for years. Here’s the medical roadmap:
- Commit to a Quit Date: Choose a date within the next 2 weeks. Mark it clearly.
- Tell Your Support System: Inform family, friends, and colleagues. Their support is invaluable. Consider joining a support group.
- Identify & Avoid Triggers: Recognize situations (morning coffee, stress, socializing) that trigger cravings and plan alternatives.
- Consider Evidence-Based Cessation Aids (Discuss with your Doctor FIRST):
- Nicotine Replacement Therapy (NRT): Provides controlled nicotine without the other toxins, easing withdrawal. Options include patches (steady dose), gum, lozenges, inhalers, nasal spray (for acute cravings). Can often be combined (e.g., patch + gum).
- Prescription Medications:
- Varenicline (Chantix): Blocks nicotine’s effects on the brain, reduces pleasure from smoking, and eases withdrawal.
- Bupropion (Zyban): An antidepressant that reduces nicotine cravings and withdrawal symptoms.
- Behavioral Therapy/Counseling: Highly effective, especially combined with medication. Teaches coping skills, stress management, and problem-solving strategies to overcome addiction. Available individually, in groups, or via phone quitlines (e.g., 1-800-QUIT-NOW in the US).
- Manage Withdrawal & Cravings:
- Delay: Urges typically peak within 5–10 minutes. Distract yourself.
- Deep Breathing: Calms the nervous system.
- Drink Water: Helps flush toxins and keeps hands/mouth busy.
- Physical Activity: Reduces cravings and stress.
- Avoid “Just One”: It almost always leads back to regular smoking.
- Prepare for Relapse: Slips happen. Don’t see it as failure. Analyze what triggered it, learn from it, and recommit immediately. Most successful quitters have made several attempts.

The Doctor’s Verdict: Your Healthiest Journey Begins Here
The medical evidence is unequivocal: smoking is a primary driver of preventable death and disability worldwide. It ravages nearly every organ system, stealing years of life and quality of life. However, the human body possesses an incredible capacity to heal once the assault of tobacco ceases.
Quitting smoking is a profound act of self-care. It requires commitment, often support, and sometimes medical assistance, but the rewards – easier breathing, a stronger heart, more energy, a brighter future, and the freedom to travel without being tethered to an addiction – are immeasurable. You don’t have to walk this path alone. Consult your doctor today. Together, you can develop a personalized quit plan tailored to your needs and embark on your most important journey yet: the journey to a smoke-free, healthier life.

Disclaimer:
This article provides general medical information and does not replace personalized advice from a qualified healthcare professional. Always consult your physician before starting any cessation program or medication.
Dr. Mohammad Rizwan Feroz


