Forget sterile waiting rooms and astronomical bills. Imagine recovering from knee surgery overlooking the turquoise Persian Gulf, or exploring ancient souks between dental check-ups. This is the evolving reality of medical tourism in the Middle East – a region rapidly transforming into a global healthcare destination. But is this surge a genuine boon for patients and economies, or does it mask potential burdens? Let’s unpack the scalpel-sharp truth.

The Allure: Why Patients are Flocking East
The Middle East isn’t just about oil riches anymore; it’s investing heavily in “healthcare cities” and world-class facilities. Countries like the UAE, Saudi Arabia, Jordan, Turkey, and Iran are leading the charge, offering compelling advantages:
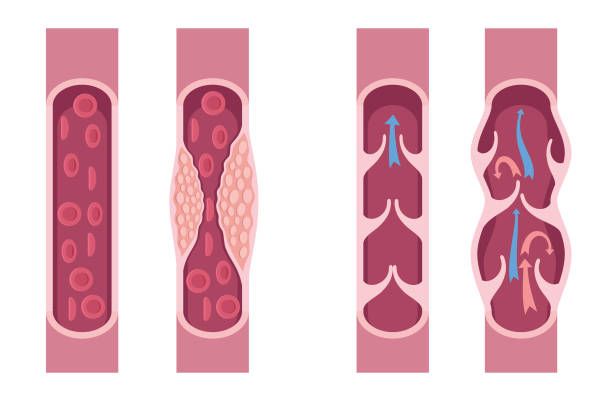
- Cutting-Edge Technology & Expertise: State-of-the-art hospitals (often branches of renowned names like Cleveland Clinic, Johns Hopkins Medicine International in Abu Dhabi) boast the latest robotic surgery systems, advanced imaging, and specialized centers for oncology, cardiology, orthopedics, and fertility. Many doctors are Western-trained, bringing international expertise.
- Cost Savings (Significant for Some): Compared to the US, UK, or even parts of Europe, complex procedures like cardiac surgery, joint replacements, or advanced dental work can cost 30-70% less, even factoring in travel and accommodation. This makes life-changing treatments accessible.
- Luxury & Hospitality: The Middle East excels at high-end service. Many medical tourism packages include 5-star recovery suites, private nurses, concierge services arranging airport transfers and leisure activities. Recovery feels more like a resort vacation.
- Reduced Wait Times: Escaping lengthy waiting lists for elective surgeries in public healthcare systems (common in Canada, UK, parts of Europe) is a major driver. Patients can often schedule procedures within weeks.
- Cultural & Religious Familiarity: For patients from the wider Muslim world and diaspora, the Middle East offers an environment sensitive to cultural norms, dietary requirements (halal food), prayer facilities, and often, staff speaking their native language. This provides significant comfort during a vulnerable time.

Meet Aisha: A Jordanian-American woman facing a year-long wait for a crucial hip replacement in the US. Drawn by familiarity, renowned surgeons, and a cost saving of nearly 50% including a luxury recovery stay, she chose a top hospital in Dubai.
“It wasn’t just the surgery,” she shared, “it was being understood, cared for culturally, and recovering somewhere peaceful. It felt like healing on my terms.”

The Thorny Side: Potential Burdens to Consider
Despite the shiny allure, medical tourism isn’t without its complexities and risks. Potential burdens lurk beneath the surface:
- Quality & Regulation Variability: While flagship hospitals are exceptional, quality and regulation standards vary significantly across the region and even within countries. Thorough research is non-negotiable. Not every “international” hospital meets the same rigorous standards.
- The Follow-Up Care Conundrum: What happens when you fly home? Coordinating post-operative care with your home doctor can be challenging. Complications arising weeks later become your local healthcare system’s responsibility, potentially causing friction or gaps in care continuity.
- Hidden Costs & Logistical Hurdles: Travel expenses (flights, visas, extended stays for recovery), unexpected complications requiring longer hospitalization, or the need for a companion’s travel can quickly erode initial cost savings. Navigating foreign bureaucracies and healthcare systems adds stress.
- Ethical Concerns & Transparency: Issues like organ transplant tourism (with its dark underbelly of trafficking and exploitation, though heavily cracked down upon), lack of price transparency in some facilities, and potential language barriers in informed consent processes raise ethical red flags that demand vigilance.
- Impact on Local Populations: Critics argue a focus on lucrative medical tourism could divert resources and top talent away from public healthcare systems, potentially exacerbating inequalities for local citizens needing care. Is the local infrastructure truly benefiting?
- Medical-Legal Recourse: Seeking legal recourse for malpractice in a foreign country is often complex, expensive, and faces significant jurisdictional hurdles. Patients may have far less protection than in their home countries.

Dr. Hassan, a leading orthopedic surgeon in Riyadh, acknowledges the challenges: “We offer world-class care, but patient selection and education are paramount. We insist on comprehensive pre-travel consultations and clear, signed agreements regarding follow-up plans with their home physicians. Transparency is key to avoiding burdens.”
Boon or Burden? The Verdict is Nuanced
Labeling Middle Eastern medical tourism solely a “boon” or “burden” is overly simplistic. It’s both, simultaneously. Its success as a boon hinges entirely on:
- Informed Decisions: Patients must meticulously research facilities (look for JCI accreditation – Joint Commission International – as a baseline), surgeons, costs, and understand all risks. DoctorTravelLog recommends verified platforms and direct consultations.
- Robust Planning: Seamless coordination between the overseas hospital, the patient, and their home healthcare provider before, during, and after treatment is critical.
- Choosing Reputable Providers: Opting for established hospitals with transparent practices and international partnerships significantly mitigates risks.
- Realistic Expectations: Understanding that while cost savings are possible, luxury packages add expense, and unforeseen complications can occur.
For the Middle East, it’s a powerful economic boon, driving investment, creating jobs, and diversifying economies beyond oil. For the right patient – well-informed, choosing accredited facilities, with a solid follow-up plan – it can be a life-enhancing, even life-saving, boon offering quality care, cultural comfort, and significant value.
For the unprepared patient or one chasing only the lowest price without due diligence, the risks can quickly transform the journey into a significant burden.
The Future: Towards Sustainable Healing
The trajectory points towards growth. Countries like Saudi Arabia (Vision 2030) and the UAE are pouring billions into healthcare infrastructure and digital health records to facilitate seamless international patient care. The focus must be on sustainable, ethical, and patient-centered development – ensuring quality is universal, regulations are stringent and enforced, benefits extend to local populations, and patients are empowered with knowledge.

Your Healing Journey?
Is the Middle East calling you for healthcare? The potential for a positive, transformative experience is real. But approach it with the same diligence you would any major medical decision. Research relentlessly, ask tough questions, prioritize accredited providers, plan your aftercare meticulously, and understand both the gleaming promise and the potential pitfalls.
Considering medical tourism in the Middle East? Share your thoughts, questions, or experiences in the comments below! Stay tuned to DoctorTravelLog for in-depth country guides, hospital reviews, and expert interviews to navigate your healthcare journey abroad safely and successfully.
Dr. Mohammad Rizwan Feroz
👍 Found this helpful? Show some love & follow us on Instagram @doctortravellog for expert tips & fresh updates!
💬 Got thoughts or questions? React below or drop a quick comment — no login needed!
❤️ 😮 🤔 👍 👎