How Regional Escalations Are Affecting Civilians and Global Travelers
Introduction
The intensifying conflict between Israel and regional actors in 2025 has reverberated far beyond military targets, triggering severe humanitarian crises and complex travel challenges. For health-conscious travelers and medical professionals monitoring global risks, understanding these interconnected impacts—civilian casualties, collapsing health systems, and logistical disruptions—is critical.
1. Civilian Casualties: The Human Toll
- Gaza: Over 38,000 reported fatalities (WHO, June 2025), including 14,500+ children. Critical shortages of ambulances, blood supplies, and morgue capacity persist.
- Lebanon: Cross-border strikes have killed 300+ civilians and displaced 100,000+ (UNOCHA), straining host communities.
- Red Sea Region: Missile attacks on shipping routes have resulted in crew injuries, maritime evacuations, and seafarer trauma.
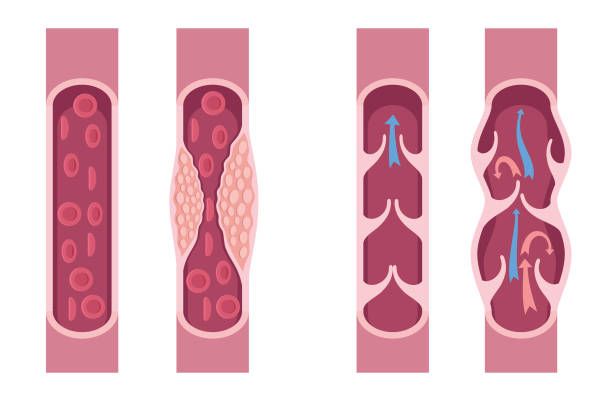
Health Implication: Mass casualties overwhelm local clinics, forcing “triage-by-survival-likelihood” in Gaza. Preventable deaths from infections, chronic conditions, and childbirth complications skyrocket.

2. Public Health Systems in Collapse
- Gaza: 90% of hospitals are non-functional (WHO). Disease outbreaks (cholera, hepatitis A) thrive amid rubble, sewage contamination, and 3L/day water access (vs. WHO’s 15L minimum).
- Lebanon/Jordan: Refugee camps face cholera and measles resurgences. Mental health crises—PTSD, anxiety—go untreated.
- Yemen/Iraq: Spillover disruptions delay medicine imports, worsening existing humanitarian emergencies.
Travel Risk: Humanitarian workers report supply shortages of antibiotics, anesthetics, and vaccines. Medical tourism to the region has halted entirely.

3. Travel in Turmoil: Borders, Flights & Insurance
- Flight Disruptions: Ben Gurion Airport (Tel Aviv) operates intermittently. Royal Jordanian, Emirates, and Turkish Airlines reroute flights avoiding Iranian/Iraqi airspace, adding 3–6 hours to EU-Asia trips.
- Border Closures: Egypt’s Rafah crossing opens sporadically. Jordan suspended visa-on-arrival for conflict-zone evacuees.
- Insurance & Costs: Most insurers void coverage for Israel, Lebanon, Yemen, Iraq, and parts of Jordan. Emergency medical evacuation (e.g., from Cyprus) now exceeds $200,000.
- Shipping Delays: Red Sea diversions add 2–3 weeks to Asia-Europe cargo, disrupting medical supply chains globally.

4. Psychological Trauma: The Invisible Crisis
- Local populations exhibit widespread symptoms of “toxic stress” (UNICEF).
- Aid workers and journalists face burnout and moral injury.
- Travelers report anxiety over regional instability, canceling trips to Türkiye, Egypt, or Jordan due to proximity fears.

DoctorTravelLog Advisory
1. Pre-Travel Planning:
- Avoid non-essential travel to Israel, Lebanon, Yemen, Iraq, and Gaza-border regions.
- Verify insurance covers conflict zones (specialized providers required).
2. Health Precautions:
- Pack trauma kits, water purifiers, and 4-week medicine supplies if working near crisis zones.
- Update cholera/hepatitis A vaccinations.
3. Ethical Travel:
- Support certified NGOs (e.g., MSF, IRC) if providing medical aid.
- Respect local trauma: Avoid photography in displacement camps.
Conclusion
The human cost of conflict extends beyond headlines—into overwhelmed hospitals, displacement camps, and the psyche of survivors. For travelers, vigilance and compassion are paramount. As borders harden and health systems fracture, the healing of nations begins with unwavering global attention to their suffering.
Stay informed with DoctorTravelLog’s real-time conflict-zone advisories.
Sources (for verification):
- WHO Situation Reports (Gaza, Lebanon)
- UNOCHA Humanitarian Bulletins
- International Committee of the Red Cross (ICRC)
- Flight disruption data: OAG, Flightradar24
- Insurance guidelines: Global Underwriters
Dr. Mohammad Rizwan Feroz / DoctorTravelLog